About 16 years ago, Sergey Menis was volunteering at a protein design lab during the day and parking cars at night. He'd come to the Baker Lab in Seattle on a whim. While earning his master's degree in bioinformatics at Chalmers University of Technology in Sweden, he read a 2003 paper describing the lab's work designing a novel protein that didn't exist in nature.
"I was just in awe of that power," Menis recalled. He wanted to learn more about biochemist David Baker's work and emailed asking to join the lab, which is based at the University of Washington. Once there, he opted to work with Bill Schief, a postdoctoral researcher with Baker who was just starting his own lab. But Schief noticed Menis wasn't fully present in his work — he often seemed sleepy. What was going on?
Menis explained about the night job at the car park. He wanted to do more at the lab, but after all, he had to pay rent. Schief asked how much Menis needed to cover his expenses. Then he hired him.
That job was a turning point.
Schief and his team, along with Menis, developed a breakthrough approach to a vaccine for HIV. In February 2021, the nonprofit scientific research organizations IAVI and Scripps Research announced exciting results in a phase 1 clinical trial — called IAVI G001 — of the Schief lab's vaccine candidate. A phase I trial represents the first time a vaccine is tested in humans, one step in what is typically a four-phase process that determines its safety, efficacy, and proper dosage. In this case, the promising vaccine produced the desired immune response in 97% of participants.
Earlier this year, building on those results, IAVI and Moderna announced that first doses had been administered in a new clinical trial of the experimental HIV vaccine. IAVI officials noted this portion of the phase 1 trial, called IAVI G002, will test the ability to prime and further mature the desired immune response using Moderna’s messenger RNA (mRNA) delivery platform used for their coronavirus vaccines. The mRNA platform enables rapid vaccine production that may dramatically accelerate the development timeline.
Guided by curiosity
Menis, who joined Amazon as a scientist in November 2020 and is now a solution architect with Amazon Web Services (AWS), hadn't set out to be a biomedical researcher, or even a scientist. "I never had a career in mind, in general," he said. "I would just follow whatever looked interesting."
As an undergrad at the University of Florida, that meant computer science. It wasn't until he had obtained his master's degree in software engineering and begun working at the defense and aerospace company Lockheed Martin that he started to rethink his career path.
Writing software for government contract projects was fine, but it didn't feel hands-on enough. "I wanted to see more feedback and results, faster," Menis said.
He recalled a bioinformatics elective class that he'd taken while in grad school at the University of Central Florida. On another fateful impulse, he decided to look at bioinformatics grad programs; this time in Europe, as he was in search of a change of scenery. He got accepted to Chalmers University of Technology and, without knowing much about the university, headed to Sweden.
"Even though it's a well-known school in certain circles, I wasn't even sure it was a real school until I arrived there," he said, laughing. "But it turned out to be a fantastic school and a really intense program."
And when he read about David Baker's work in inventing a protein molecule from scratch, the next chapter of his career — computational protein design — began to unfold.
HIV: a formidable foe
Human immunodeficiency virus has infected more than 75 million people and killed more than 32 million since the epidemic began in early 1980s. With the isolation of the virus in the mid-1980s, it seemed that a vaccine was in the offing. But conventional approaches, which involve taking some inactivated part of the virus to stimulate an immune response, have not worked for HIV.
The virus has multiple wily strategies it employs to hide within the body. It cloaks itself with sugars that make it nearly invisible to the human immune system. And its surface is always changing, a series of disguises that fool most enemy antibodies. But researchers have identified a ray of hope buried within the immune system: the potential to make bnAbs, which can recognize and defeat 99% of HIV strains.
The problem is, people don't develop bnAbs until they're years into an infection. “That's too little, too late," Menis said. "By the time you've actually started developing the responses you need, you're already productively infected."
The strategy researchers are pursuing is to initiate the process of making these potent antibodies before infection occurs, giving the body a head start. To do so, they must identify the right "baby antibodies," as Menis calls them, and train them to be bnAbs.
Given that the human body has the ability to make an estimated 1 quintillion unique antibodies, finding and training the right ones is a needle-in-the-haystack endeavor. And only certain antibodies have the ability to become bnAbs—those baby antibodies are literally one in a million.
Only a small fraction of people with HIV develop the most potent bnAb response — the kind an effective vaccine would elicit — on their own. Researchers have been able to zero in on these antibodies by analyzing blood from HIV-positive donors. But there's good news, and the recent clinical trial confirmed it.
"Nearly everyone in the world should have the cells needed to start the process of producing this immune response," Menis said. "To get that process started, we need to find them, stimulate them, and have them multiply."
Building a vaccine platform
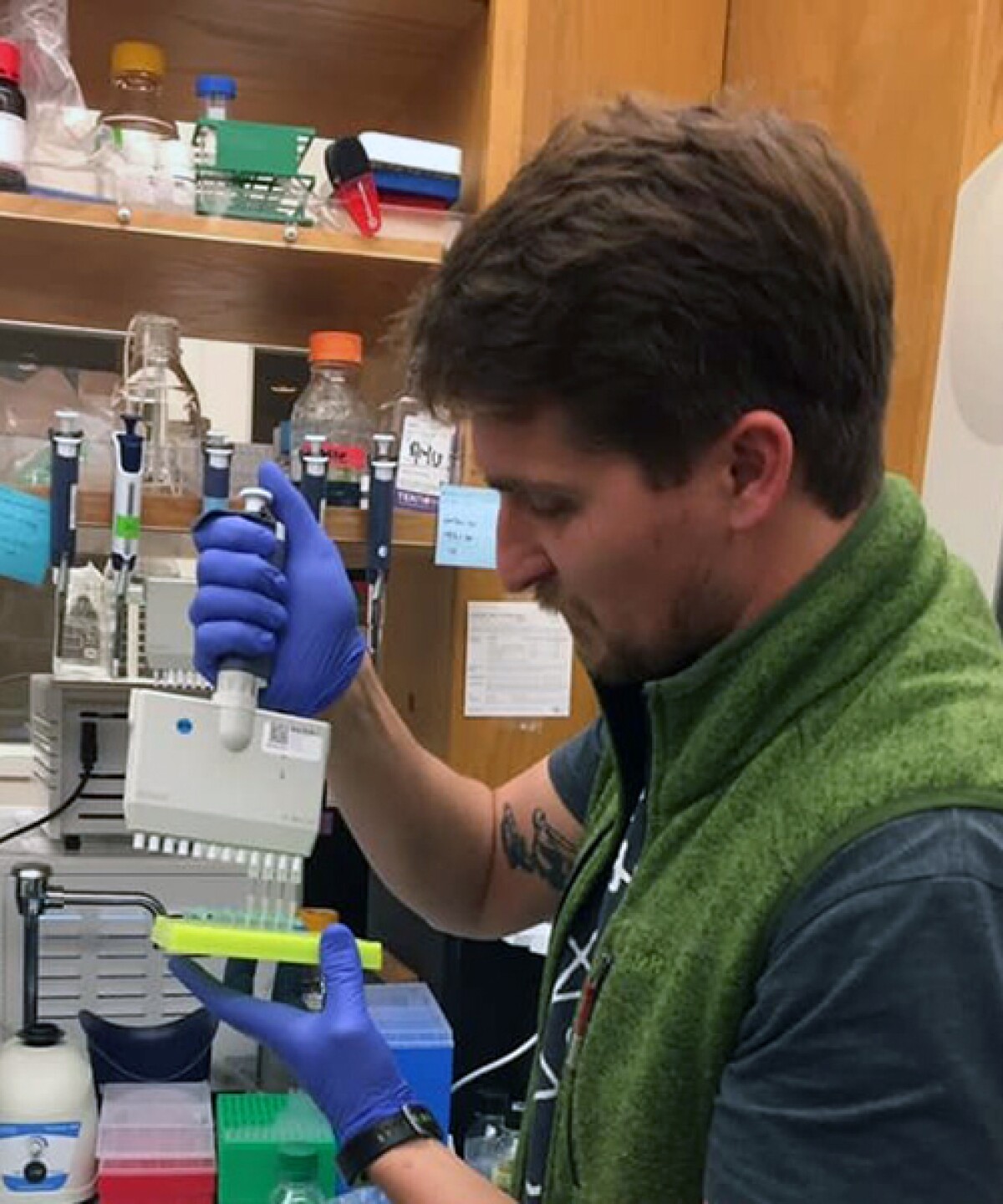
After Menis began working at Baker Lab, he decided to pursue a PhD in biochemistry at the University of Washington in the Schief lab. Menis moved to San Diego midway through his PhD studies when Schief moved his lab to Scripps Research and IAVI.
"Sergey is very thoughtful and calm, with meticulous attention to detail. He is curious about how things work," said Schief, who is executive director of vaccine design for IAVI’s Neutralizing Antibody Center (NAC) at Scripps Research and a professor in the Department of Immunology and Microbiology at Scripps.
Schief advised Menis on his PhD thesis, during which Menis developed the nanoparticle platform that underpins the HIV vaccine candidate. The nanoparticle Menis designed snaps together with a protein, eOD-GT8, which is optimized to stimulate production of the rare antibodies that can eventually become bnAbs. The eOD-GT8 protein was developed primarily by another PhD student in the Schief lab, Joe Jardine. The nanoparticle amplifies the body's response by delivering multiple copies of eOD-GT8.
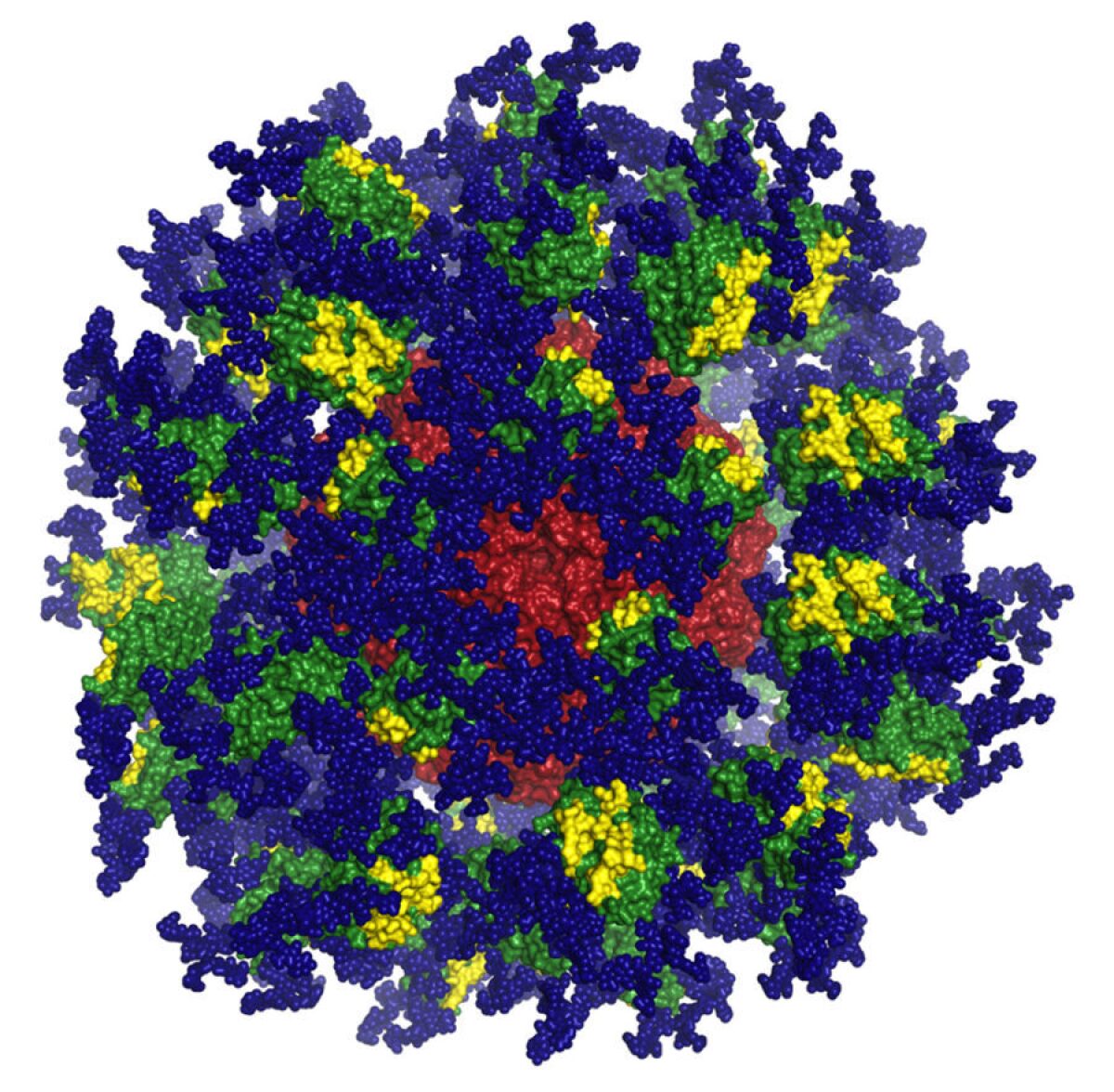
"It's spherical, like a virus, so the immune system treats it as if it might be a virus of some kind," Menis said. "We want to make it look like a little virus, even though it has no infectious properties whatsoever."
Menis served as the Schief lab's subject matter expert during the multi-year process of developing the vaccine candidate. "He played a big role in planning and carrying out the clinical trial," Schief said.
A team effort
Both Menis and Schief are careful to emphasize that there is much more to do before an approved HIV vaccine becomes reality. While the results from IAVI G001 are encouraging, there are significant milestones remaining.
"By demonstrating that this concept works in humans, and actually can work very well in terms of eliciting strong and consistent responses of the kind we wanted, I hope we have accelerated HIV vaccine development by providing findings that we and others can build on," Schief said.
Menis is also quick to credit the 48 volunteers who participated in the IAVI G001 clinical trial, noting that without such volunteers, a vaccine wouldn’t be possible. "They are the co-creators of this effort," he said. Schief and Menis also praised the work of many other individuals, particularly colleagues at Fred Hutch, George Washington University, and the NIH Vaccine Research Center.
The upcoming IAVI G002 will recruit 56 volunteers across four sites: GWU School of Medicine and Health, Hope Clinic of Emory Vaccine Center in Atlanta, Fred Hutchinson Cancer Research Center in Seattle, and the University of Texas–Health Science Center at San Antonio. The goal: replicate the priming of “baby antibodies” observed in IAVI G001 and teach them to take a step towards becoming a bnAb capable of neutralizing HIV.
An intriguing offer
Menis was working at IAVI and preparing to go on vacation when Amazon contacted him in 2020, asking whether he'd be interested in a position at the company. The hiring process happened quickly: He did an interview while on the trip, and on his first day back from vacation, he had an offer in his inbox.
"When Amazon reached out, I was really intrigued by the possibilities of what a giant like Amazon could be doing," Menis said. "I was open to discovering what that meant."
After spending a little over a year as a research scientist, Menis moved into a senior product manager role with Amazon Diagnostics and then transitioned into a role as a solution architect with AWS, building solutions for healthcare and life sciences startups. “For me, the roles represent opportunities to learn and be curious,” Menis said, citing one of Amazon’s leadership principles.
He admitted he didn’t know much about the principles until his first job interview, but now he has come to appreciate them. He enjoys seeing how they relate to him and his past work.
“Working at Amazon has been a learning experience,” he says — yet another on the journey from lab volunteer to medical-breakthrough-creating scientist to whatever the next chapter will be.










